Though the idea of stroke may be daunting, knowing the link to birth control and being aware of your risk factors gives you control over making choices regarding your health. Read ahead to know more!
For millions of women, birth control is a reliable method of contraception and management of reproductive health.
But a question that often surfaces, sometimes with frightening headlines, is whether or not hormonal birth control raises the risk of stroke. Although the overall risk is low in most healthy people, it’s an important discussion to have with your medical care provider.
The Oestrogen Link: Why Some Birth Control Raises Concerns
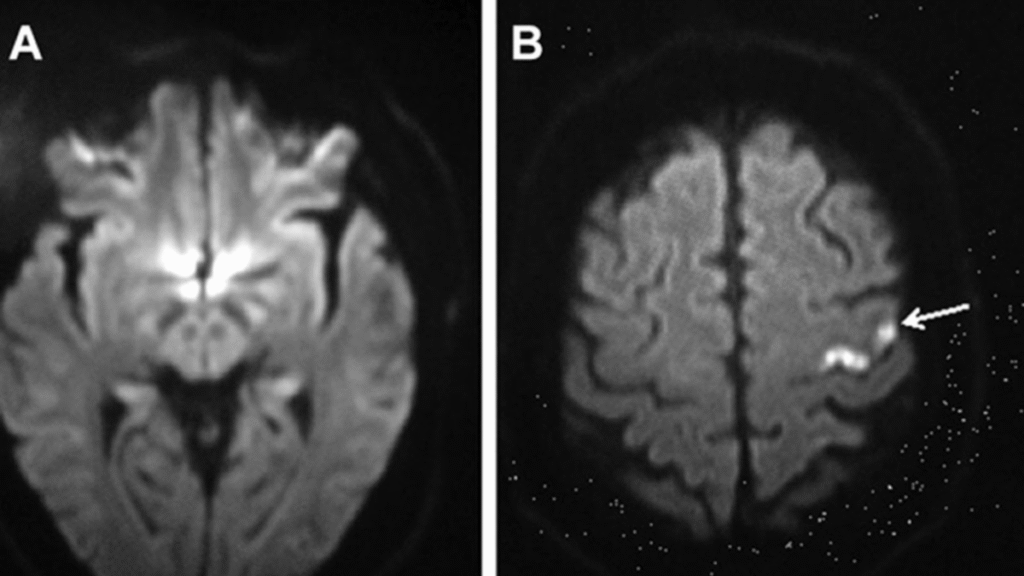
In an exclusive interaction with the editorial team of Onlymyhealth, Dr Vikas Yadav, Senior Consultant, Department of Obstetrics, Gynecology & IVF Specialist, ShardaCare, Healthcity – Noida, explained that the major offender behind the risk of stroke seen with some methods of birth control is oestrogen, especially in the case of combination oral contraceptive pills, patches, and vaginal rings. Oestrogen can affect proteins responsible for blood clotting in the body, and can thereby enhance the tendency of the blood to clot. “When a clot develops in a blood vessel that serves the brain, it can cause an ischemic stroke, the most frequent form of stroke,” Dr Yadav pointed out.
“Worth noting here is that the doses of oestrogen in current birth control are much lower than those employed decades earlier, which accounts for the decreased overall risk compared to older models of the pill,” he added.
Who is at Higher Risk? Identifying Key Factors
Although the overall risk for stroke among healthy women on oestrogen-based birth control is low (approximately 8 per 100,000 individuals), pre-existing conditions as well as lifestyle characteristics can dramatically increase it. According to Dr Yadav these include:
35 years and older, particularly with smoking: This combination itself is a big red flag since both age and smoking each raise the risk for stroke.
History of high blood pressure (hypertension): Uncontrolled hypertension is a major stroke risk factor.
History of blood clotting disorders: People with an inclination to form blood clots should usually not take estrogen-containing birth control.
Migraines with aura: This is a very significant consideration. Women who have migraines with visual symptoms (aura), numbness, or other neurological symptoms are at an increased risk for stroke, and this risk is even greater with estrogen-containing birth control.
History of prior stroke or transient ischemic attack (TIA): If you’ve had a stroke or TIA, estrogen-containing birth control is usually contraindicated.
Diabetes, hyperlipidemia, or obesity: These states also add to overall cardiovascular risk and are sometimes worsened by estrogen.

Knowing the Warning Signs: Act F.A.S.T.
No matter what your method of birth control, it’s important to know the signs of a stroke. Immediate medical care is essential, since “time lost is brain lost.”Dr Yadav also elucidated on the F.A.S.T. acronym:
F: Drooping of one face: Does one side of the face sag or feel numb? Have the person smile.
A: Weakness in one arm: Is one arm weak or numb? Have the person lift both arms. Does one arm fall downward?
S: Difficulty with speech: Is speech slurred, or is the person unable to talk or difficult to understand? Have the person repeat a simple sentence.
T: Time to visit a doctor: If you see any of these signs, even when they disappear, call emergency services at once.
Other stroke symptoms that women might have, besides the classic ones, include sudden hiccups, nausea, pain in the chest, weakness, shortness of breath, and palpitations.
“Therefore, the choice of which method of birth control is appropriate for you should always be made in close discussion with your healthcare provider. They will get a comprehensive medical history, including any pre-existing medical conditions, lifestyle factors, and family history of stroke or blood clot,” Dr Yadav noted.
Bottomline
Though the idea of stroke may be daunting, knowing the link to birth control and being aware of your risk factors gives you control over making choices regarding your health. Only after close coordination with your physician should you identify and adopt an effective and safe treatment for yourself.











2 thoughts on “Is Your Birth Control Putting You at Risk for Stroke? Expert Weighs In”